Post-Infectious IBS: Upset Tummy Weeks After a Stomach Bug?
Irritable Bowel Syndrome (IBS) is a functional gut disorder that affects 1 in every 7 people, or 15% of the world population, where 2/3 of treatment seekers are women. IBS is characterised by chronic, relapsing symptoms including lower abdominal pain and discomfort, bloating, wind, and altered bowel habits - ranging from diarrhoea to constipation.
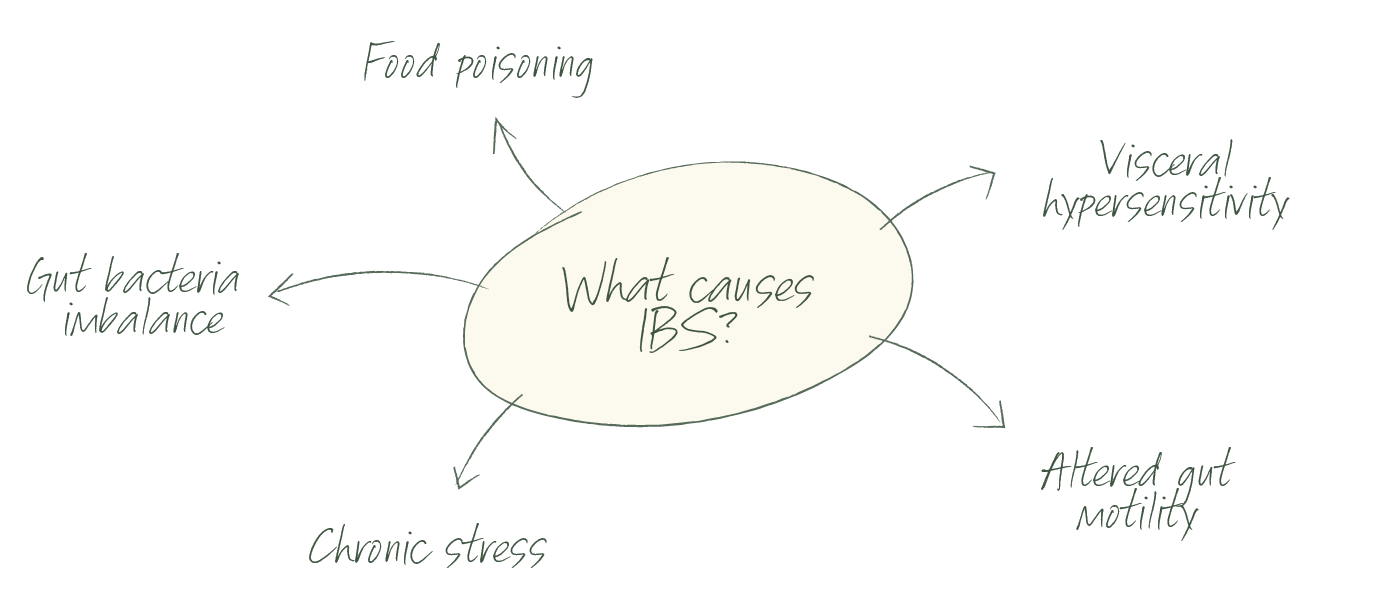
What Causes Irritable Bowel Syndrome (IBS)?
The exact cause of IBS is not well understood, but it is believed to result from a combination of factors including:
Infections such as gastroenteritis (aka stomach bug)
Hypersensitivity to pain from within the bowel
Psychosocial factors like stress
An imbalance of gut bacteria also known as dysbiosis
Altered gastrointestinal motility
What is Post-Infectious IBS?
Post-Infectious IBS is a form of IBS that is caused by food poisoning (aka stomach bug). Although not much is talked about, 1 in every 9 people who experience food poisoning happen to develop Post-Infectious IBS up to six months after the initial bacterial infection. Post-infectious IBS almost always has a diarrhoeal component, a hallmark symptom of traveller’s diarrhoea and gastroenteritis.
How does food poisoning cause IBS?
The most common bacteria that cause food poisoning - Salmonella, E.Coli, Campylobacter and Shigella, release a toxin called Cytolethal Distending Toxin B (CdtB). When CdtB enters the body, the immune system fights back with an antibody called anti-CdtB. Due to molecular similarities, CdtB looks similar to vinculin, a naturally occurring protein in the body that is critical for normal gut function. Because of this similarity, the immune system gets confused and thinks it needs to fight back against vinculin and starts to produce another antibody, called anti-vinculin. The production of anti-vinculin antibodies leads to gut nerve damage and improper functioning of the Interstitial Cells of Cajal (ICC) and the Migrating Motor Complex (MMC) - both play a critical role in gut motility. As a result, gut motility is impaired and bacteria starts to accumulate in the small intestine leading to the development of Small Intestinal Bacterial Overgrowth (SIBO).
How is Post-Infectious IBS diagnosed?
Until recently IBS was a diagnosis of exclusion, meaning that GPs and medical specialists would rule out any medical condition such as Inflammatory Bowel Disease, Coeliac Disease and most recently Endometriosis, before concluding your digestive symptoms are caused by IBS.
It is of course of extreme importance to go through this process to make sure nothing more serious is going on, and if you get cleared from any medical condition and think your digestive symptoms started after an episode of food poisoning/gastroenteritis, you are a strong candidate to have developed Post-Infectious IBS.
Post-infectious IBS is the only form of IBS that has a diagnosis test called IBS Smart - a blood test developed in the USA by world leading IBS researcher Dr. Mark Pimentel, that measures the levels of two validated IBS biomarkers, anti-CdtB and anti-vinculin, providing a positive or negative result. If the measured biomarkers are elevated, it is then confirmed that your IBS developed from food poisoning/gastroenteritis.
What is Small Intestinal Bacterial Overgrowth (SIBO)?
SIBO stands for Small Intestinal Bacterial Overgrowth, that means there is an accumulation of bacteria in the small intestine. These bacteria normally live in our gastrointestinal tract, more precisely in the large intestine, but have overgrown in a location not meant to host so many bacteria. That becomes a problem because bacteria ferment dietary fibre and gas is produced as a result of this fermentation - when SIBO occurs, the accumulation of gas in the small intestine results in bloating, flatulence, abdominal distension, abdominal pain and altered bowel movements. Although food poisoning is the most common root cause of SIBO, many other health conditions have been associated with it.
How is SIBO diagnosed?
SIBO is diagnosed via a breath test. The test measures hydrogen and methane, or hydrogen sulphide gases, which are exclusively produced by gut bacteria and exhaled in our breath.
IBS-SIBO Connection
SIBO and IBS are separate conditions, but they commonly coexist. That means that if you have been diagnosed with IBS, there is a strong likelihood that you may have SIBO as well. A study found that of 202 irritable bowel syndrome patients, 157 (78%) had bacterial overgrowth and eliminating it improved IBS symptoms in 48% of them.
Of 202 IBS patients, 157 (78%) had bacterial overgrowth.
Eliminating it improved IBS symptoms in 48% of them.
IBS-SIBO Management
Food poisoning is just one of the many causes that lead to the development of IBS, it is widely known that stress and anxiety are triggers for some individuals. Regardless of what triggered your IBS symptoms, a multifactorial approach is needed to keep them at bay while working on the underlying cause(s) of why you experience them in the first place.
If you are struggling with chronic digestive symptoms, get in touch! I have personally experienced the consequences of post-infectious IBS and SIBO. During my long and painful journey towards better gut health, I have gained extensive knowledge and a deep interest in digestive health, and my desire to help others lead me to qualify as a nutritional therapist specialising in SIBO and IBS.
Written by Marilia Chamon
Registered Nutritional Therapist, Gut Health, IBS & SIBO Expert
Founder of Gutfulness Nutrition
Instagram @gutfulnessnutrition